By The Mortenson Portland Healthcare Team
The Next Level of Infection Prevention & Construction Control – A Comprehensive Approach
Construction in an active healthcare facility can be risky. One of the highest risks is the potential for patient infection from construction dust leaving the project site. Just by its very nature, you have an inherently dirty process taking place in a facility with no tolerance for dirt, dust or other contaminates in patient areas. Airborne contaminants are of particular concern as they are the most challenging to contain. Special care needs to be taken to ensure surrounding areas remain clean while renovations are taking place, regardless of if the area is considered sterile or not. Below, we’ll walk you through some examples of the physical and procedural controls we have put in place on previous projects to help mitigate these concerns.
Collaboration
The first step in the process is creating a collaborative environment with the right stakeholders to ensure a contamination control plan is comprehensive. This typically involves the participation of end users, architects, engineers, contractors, and facilities staff. Ideally this collaborative team is formed during the programming or schematic phase of design so that the contractor and facilities staff can provide information which influences design. This way the users can have a full understanding of what the plan is, where the work is taking place, how the work will progress and what the impacts will be. If any issues are identified at the programming level, it is quicker and less costly to make adjustments early rather than after construction is underway. The earlier the concerns can be identified, the better.
Temp Barrier Plan
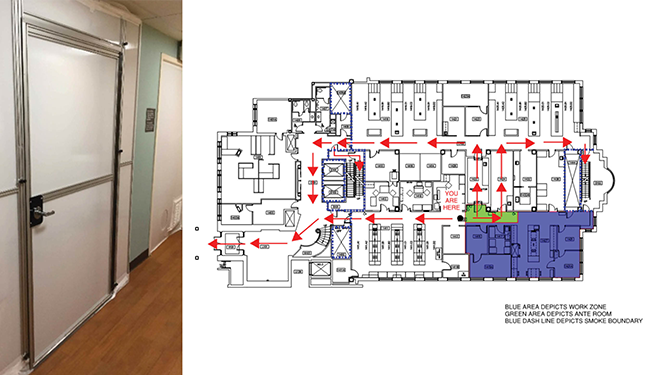
The first deliverable the team will need to compile in relation to infection control risk mitigation is the temporary barrier outline. This typically consists of a marked-up floorplan in the demolition phase indicating the temporary barrier locations. Depending on the phasing of the project, additional markups will be needed as the project is built out and the environment changes. Another item outlined in this plan is the type of temporary barrier to be utilized, which is dependent on project duration, surrounding hospital operations, facility preferences, front or back of house, and phasing needs. One simple solution typically used in short duration projects is hanging plastic to isolate the area. Other solutions may include building a hard barrier. Some examples are shown below. The last item to consider when planning out a temporary barrier plan is what to do above the ceiling. Typically, a construction project will need to remove a portion of the ceiling to tie into existing facility systems. When the ceiling is removed, the barrier in place needs to reach the next highest point which is typically the deck for the floor or roof above. The best way to seal this space above the ceiling is typically draping plastic to ensure an airtight seal.
Another item to note is whether an anteroom is needed between the construction space and the clean space. This decision will be based on the project scope and the impact to adjacent operations. An anteroom is a separate sealed area where workers can ensure no dust is contaminating their clothing, tools or materials before leaving the construction space.
Negative Air Plan
One of the best ways to control unwanted contaminants from entering or exiting a space is by manipulating air pressures. If you have a non-sterile space (construction area) with a low air pressure and a sterile space (patient area) with a higher pressure the air pressures will move any airborne particles from the sterile space to the non-sterile space. There are multiple ways to create this pressure variation including venting to the exterior of the building, setting up temporary HEPA-filtered fans and adjusting the existing HVAC system to help accommodate airflow needs. The best way to communicate this plan is to identify where the construction space (negative area) is and where the non-construction (positive area) space is. The plan will also indicate how the team plans to create a negative air environment.
Whenever there is an existing system going through the construction space, special care is needed to ensure a contaminant is not leaving the construction space through that system. This can include HVAC systems, potable and non-potable water systems, medical gas systems, pneumatic tube systems, or any other system that has a medium leaving the construction space. There are multiple ways to stop systems from spreading contaminants, and the project team will need to work closely with the facility team, system experts and MEP trade partners to ensure the plan is implemented properly.
Inspection and Testing Plan
One of the most important procedural items relating to infection controls is the inspection, testing and documentation plan. The team needs to develop a plan that satisfies all regulatory agency needs and fits into the medical facility’s existing program. This can be as simple as verifying the space in low-risk areas has a negative air pressure compared to patient space or it can be as extensive as monitoring and recording air particle readings at the point of construction space air discharge. The facility’s infection control team along with the hospital staff will help inform the rest of the core team what the risks are and how best to mitigate them.
Fire Barriers
Another potential risk to address is the impacts to rated partitions. Whenever you alter existing walls, you must be aware of how the changes affect the fire and life safety plans in both the short and long term. Vertical penetrations through the floor or ceiling will also need to be considered. Most floors are rated barriers that must be maintained. Fire barrier risk can be mitigated by creating a fire barrier penetration plan outlining where and when these barriers will be impacted and what the temporary or final solution will be. The plan must also outline any changes in task-level operations since the work may be taking place outside of the standard construction boundary. Marking-up a floor plan that indicates locations of penetrations and any compromised fire barrier along with a brief narrative explaining the markups is the most useful way to communicate this plan.
Communication Plan
By creating the collaborative environment noted above, the team will be able to lean on industry experts to weigh in on different parts of the plan. It’s incredibly important to have open lines of communication with all parties throughout the entire project lifecycle. Early communication will help ensure everybody is on the same page to start. Regular, consistent follow-up is needed to ensure the plan is being followed and any necessary changes to the plan are captured and executed appropriately.
Closing
In a medical environment, the infection control plan must be initiated along with all the other preconstruction planning activities. When you have a highly collaborative environment with the right team members, all pertinent subject matter experts can evaluate and comment on the plan with ample time to make any adjustments before construction begins. This helps to produce a successful disruption avoidance plan. By communicating the infection control plan to the right stakeholders early in preconstruction, we can better manage expectations and ensure the medical facility operations are not negatively affected by any construction. After all, the end goal for the entire project team is to provide an outstanding experience for patients, families and staff.